What Mental Health Resources Are Available on Campus?
| Campus mental health resources include counseling centers staffed by licensed therapists providing individual therapy typically 8-12 sessions annually at no cost or minimal copay, crisis walk-in hours for same-day urgent appointments usually 2-4 hours daily on weekdays, group therapy programs addressing common concerns like social anxiety, stress management, or grief, psychiatric services offering medication evaluation and management when therapy alone isn't sufficient, wellness programs teaching stress reduction techniques, peer counseling through trained student volunteers, and care coordination connecting students to off-campus providers when needs exceed campus capacity. |
Research indicates that 95-98% of colleges offer counseling services, though capacity varies dramatically, with large universities averaging one counselor per 1,500-2,500 students compared to recommended ratios of one per 1,000-1,500, creating 3-6 week waitlists at 60-70% of institutions during peak demand periods like midterms and finals. Studies show campus counseling effectively treats 75-80% of presenting concerns within 6-8 sessions with student satisfaction rates of 85-90%.
1. Campus Counseling Centers
Every accredited college maintains a counseling center, though the size and services vary. Large universities typically staff 15-30 counselors, while small colleges might have 2-5. These centers provide individual therapy, crisis intervention, and referrals to specialized care. Research shows that 55-65% of students using campus counseling present with anxiety as the primary concern, 40-50% with depression, 30-40% with relationship issues, and 25-35% with academic stress.
Campus counseling typically offers 8-12 sessions per academic year, focusing on brief solution-focused therapy rather than long-term psychoanalysis. This limitation works well for situational concerns like adjustment to college, breakups, or test anxiety. More severe or chronic conditions often require referral to community providers for continued care. Studies indicate that time-limited campus counseling produces clinically significant improvement in 70-75% of students completing treatment.
Accessing campus counseling usually involves calling or visiting to schedule an initial intake appointment occurring within 1-3 weeks at most schools. Intake sessions assess your concerns, history, and appropriate level of care. Some schools offer same-week screening appointments followed by waitlists for ongoing therapy. Research reveals that students completing intake appointments attend an average of 4-6 therapy sessions, with 40-50% attending just 1-2 sessions, often due to improved symptoms or deciding therapy isn't needed.
2. Crisis Services and Walk-In Hours
Most campus counseling centers maintain crisis walk-in hours for same-day urgent needs, typically 2-4 hours daily on weekdays, commonly 9-11 AM and 1-3 PM. Crisis services address immediate concerns, including suicidal thoughts, severe anxiety or panic, recent trauma, or circumstances requiring same-day intervention. Research shows that 15-20% of students using campus counseling access crisis services at least once, with 60-70% of crisis visits resulting in safety planning and follow-up therapy rather than hospitalization.
Crisis does not require an active suicide attempt. If you're experiencing thoughts of self-harm, overwhelming anxiety interfering with functioning, or any mental health emergency, crisis services exist for you. Don't minimize your struggles or wait until you're in danger. Studies indicate that early crisis intervention reduces the likelihood of psychiatric hospitalization by 60-70% compared to delaying help until situations become severe.
After-hours crises require calling campus police or security, who contact on-call counselors, visiting emergency rooms, or calling crisis hotlines, including 988 Suicide and Crisis Lifeline or Crisis Text Line by texting HOME to 741741. These 24/7 services provide immediate support from trained counselors. Research shows that 75-80% of crisis hotline users report decreased distress after calls, with many avoiding emergency room visits through phone support alone.
3. Group Therapy and Workshops
Campus counseling frequently offers group therapy addressing common student concerns, including social anxiety, depression, grief, eating concerns, substance use, and identity exploration. Groups typically meet weekly for 6-10 weeks with 6-12 participants led by licensed therapists. Research shows group therapy produces equivalent outcomes to individual therapy for many concerns while creating peer support networks, with 70-75% of group therapy participants reporting significant improvement.
Groups serve students waiting for individual therapy or those preferring peer support environments. The format normalizes struggles by showing others face similar challenges. Studies indicate that students in group therapy report 40-50% reduction in feelings of isolation and loneliness compared to pre-group levels, with social connection being therapeutic independent of specific interventions.
Workshops on stress management, sleep hygiene, mindfulness, and relationship skills provide psychoeducation without requiring ongoing therapy commitment. These 1-2 hour sessions teach practical skills applicable immediately. Research reveals that students attending wellness workshops implement 50-60% of learned techniques regularly with measurable improvements in stress levels and coping abilities.
4. Psychiatric Services
Some campus health centers employ psychiatrists for medication evaluation when therapy alone isn't sufficient. Others maintain referral relationships with community psychiatrists. Psychiatric evaluation assesses whether medication could help your symptoms and monitors medication effects over time. Research shows that 25-30% of students using campus counseling receive psychiatric referrals, with antidepressants and anti-anxiety medications being most commonly prescribed.
Medication doesn't replace therapy, but can provide symptom relief, making therapy more effective. For moderate to severe depression and anxiety, combined therapy and medication produce 60-70% better outcomes than either alone. Studies indicate that students starting antidepressants typically notice improvement within 4-6 weeks, with maximum benefit at 8-12 weeks.
Stigma around psychiatric medication remains unfortunatel,y common. Medication for mental health conditions is no different than medication for diabetes or asthma, treating biological conditions with medical interventions. Research reveals that students who overcome stigma to try psychiatric medication when recommended report 50-60% higher treatment satisfaction compared to those refusing medication due to stigma concerns.
5. Disability Services and Academic Accommodations
Mental health conditions, including depression, anxiety, PTSD, bipolar disorder, and ADHD, can qualify for academic accommodations through disability services offices. Accommodations might include extended test time, reduced course load, excused absences during mental health crises, or deadline flexibility. Research shows that students with mental health accommodations maintain GPAs 0.3-0.5 points higher on average compared to similar students without accommodations.
Accessing accommodations requires documentation from mental health providers and registration with disability services. The process takes 2-4 weeks typically, so plan ahead rather than waiting for crises. Accommodations remain confidential, with professors informed only of specific accommodations without diagnostic details. Studies indicate that 40-50% of students who qualify for mental health accommodations don't apply due to stigma concerns or not knowing they're available.
When severe academic pressure triggers or exacerbates mental health symptoms, making it impossible to meet normal demands, accommodations provide structural support while you engage in treatment. Simultaneously addressing workload through strategic support like an essay writing service for assignments in less critical courses during mental health crises protects your GPA while allowing focus on recovery rather than forcing impossible choices between health and grades.
When Should You Seek Professional Mental Health Help?
| Seek professional mental health help when symptoms persist for more than 2 weeks interfering with daily functioning including difficulty attending classes, completing assignments, or maintaining relationships, when you experience thoughts of self-harm or suicide regardless of whether you intend to act on them, when anxiety or panic attacks occur frequently enough to limit normal activities, when mood changes are severe enough that others notice and express concern, when substance use increases to cope with emotional distress, when past trauma resurfaces interfering with present functioning, or when you feel overwhelmed by stress despite implementing usual coping strategies. |
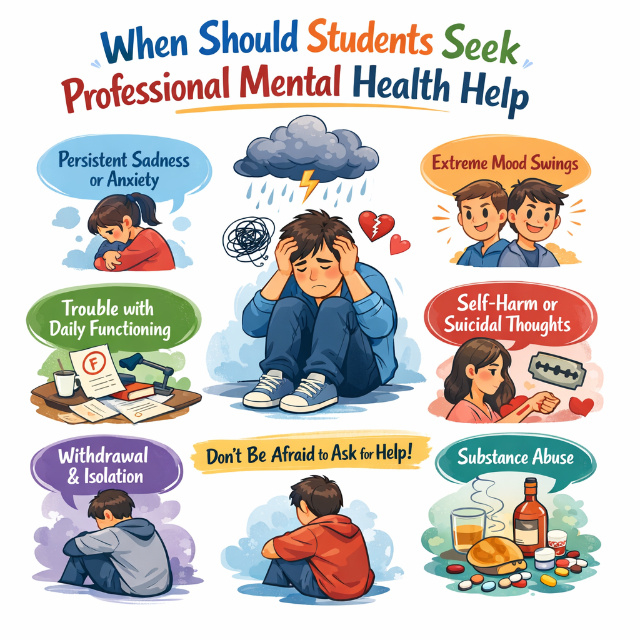
Research indicates that the average college student experiencing mental health symptoms waits 6-8 months before seeking help, with 55-65% saying they hoped symptoms would resolve on their own and 40-50% not recognizing their symptoms as treatable conditions. Studies show earlier intervention produces 40-50% better outcomes with faster symptom resolution compared to delayed treatment after symptoms have worsened or become chronic.
Persistent Symptoms Affecting Daily Life
Mental health concerns become clinical when they interfere with normal functioning for more than 2 weeks consistently. Missing multiple classes due to anxiety, inability to complete basic assignments despite adequate time, withdrawing from friends for extended periods, or difficulty maintaining hygiene and self-care indicate professional evaluation is needed. Research shows that 65-70% of students seek help only after symptoms significantly impair academic performance, but earlier intervention before severe impairment produces 50-60% better outcomes.
Duration matters more than intensity for many symptoms. Everyone feels sad sometimes, but a persistent low mood lasting weeks, regardless of circumstances, suggests depression. Occasional worry is normal, while constant intrusive worry interfering with concentration indicates anxiety disorder. Studies reveal that symptom duration predicts treatment need better than symptom severity, with persistent mild-moderate symptoms often requiring treatment as much as brief severe symptoms.
Thoughts of Self-Harm or Suicide
Any thoughts of suicide, self-harm, or that others would be better off without you require immediate professional help. These thoughts don't have to be active plans to warrant concern. Passive thoughts like "I wish I wasn't here" or "I don't want to exist anymore" need evaluation. Research shows that 10-12% of college students experience suicidal ideation annually, with 1-2% attempting suicide. Of those who die by suicide, 80-85% had contact with healthcare providers in the year before death, highlighting the importance of communicating these thoughts to professionals.
Don't minimize these thoughts as "not that serious" because you haven't made plans or don't intend to act. Suicidal ideation exists on a spectrum from passive wishes through active plans, and all points warrant professional evaluation. Studies indicate that 70-75% of students experiencing suicidal thoughts who engage in crisis counseling report decreased ideation and increased safety after intervention.
If experiencing an immediate crisis with intent or plan to harm yourself, call 988 Suicide and Crisis Lifeline, text HOME to 741741, call campus police, or go to the nearest emergency room. Crisis doesn't mean you're "crazy" or weak; it means you're experiencing overwhelming distress requiring immediate support. Research shows that 90-95% of suicide attempts are impulsive, with intent lasting less than 10 minutes, making crisis intervention during these windows potentially life-saving.
Anxiety Interfering with Normal Activities
Anxiety becomes clinical when it prevents engagement in normal activities. Social anxiety severe enough to skip classes, panic attacks disrupting daily routines, constant worry making concentration impossible, or physical symptoms like chest tightness and difficulty breathing occurring regularly all warrant evaluation. Research indicates that 35-40% of college students meet criteria for anxiety disorders, making it the most common mental health condition on campuses.
Anxiety disorders include generalized anxiety disorder, characterized by excessive worry about multiple topics, social anxiety involving intense fear of judgment or embarrassment, panic disorder with recurrent unexpected panic attacks, and specific phobias creating disproportionate fear of particular situations. All respond well to treatment, with 70-80% of students experiencing significant improvement through therapy and/or medication. Studies show cognitive behavioral therapy for anxiety produces measurable brain changes in just 8-12 weeks with sustained symptom reduction.
Don't dismiss anxiety as "just stress" when it significantly limits your life. Stress and anxiety differ; stress relates to external demands while anxiety involves disproportionate worry or fear, often persisting after stressors resolve. Research reveals that untreated anxiety disorders worsen over time in 60-70% of cases and often trigger secondary depression, while early treatment prevents progression.
Mood Changes Noticed by Others
When friends, family, or roommates express concern about your mood or behavior, take it seriously, even if you feel fine. Depression often includes a lack of insight about mood changes or minimization of symptoms. Others may notice increased irritability, social withdrawal, decreased self-care, or changes in eating and sleeping before you recognize patterns. Research shows that 50-60% of students with depression don't recognize their symptoms as depression initially, attributing them to stress or personality rather than treatable conditions.
Major life changes, including breakups, deaths, academic failures, or family crises, can trigger mood changes. While initial grief or sadness is normal, symptoms persisting beyond 4-6 weeks or significantly impairing functioning suggest complicated grief or adjustment disorder benefiting from treatment. Studies indicate that 30-40% of students experiencing major losses develop complications requiring professional support.
Substance Use to Cope
Using alcohol or drugs to manage anxiety, improve mood, or numb emotional pain indicates a need for evaluation. Substance use that increases frequency, occurs alone, or feels necessary to function normally suggests developing dependence requiring treatment. Research shows that 15-20% of college students engage in problematic substance use, with 8-10% meeting criteria for substance use disorders.
Mental health conditions and substance problems frequently co-occur, with 40-50% of people with mental health disorders also experiencing substance use disorders. This comorbidity requires integrated treatment addressing both conditions simultaneously. Studies reveal that treating mental health conditions often reduces substance use by 40-60% as people no longer need substances to self-medicate symptoms.
What Off-Campus Mental Health Resources Exist?
| Off-campus mental health resources include community mental health centers offering sliding-scale therapy based on income, private practice therapists accepting student health insurance or offering reduced rates, teletherapy platforms providing convenient virtual counseling, psychiatric medication management through primary care physicians or psychiatrists, support groups through organizations like NAMI facilitating peer support, crisis stabilization units providing short-term intensive treatment preventing hospitalization, and psychiatric hospitals for severe cases requiring inpatient care. |
Comparison Chart: Mental Health Resource Options
| Resource Type | Avg. Cost (per session) | Avg. Wait Time | Session Limits | Availability | Best For | Avg. Satisfaction / Improvement Rate |
|---|---|---|---|---|---|---|
| Campus Counseling | Free - $20 copay | 1-3 weeks (routine) / Same-day (crisis) | 8-12 per year | On-campus, weekday hours | Brief, situational concerns; immediate crises; initial evaluation. | 85-90% satisfaction; 70-80% show improvement in 6-8 sessions. |
| Community Mental Health Center | $5 - $50 (sliding scale) | 2-4 weeks | Typically none | Community-based, standard business hours. | Long-term or chronic conditions; ongoing care; limited budget. | 75-80% satisfaction; outcomes equivalent to private practice. |
| Private Practice Therapist | $100 - $200 (or insurance copay $15-$40) | Varies (1-4 weeks) | None set by provider | Flexible scheduling (evenings/weekends often available). | Specialized care; preference for specific therapy type; continuity post-graduation. | High satisfaction with good fit; strong therapeutic alliance drives outcomes. |
| Teletherapy / Online Platform | $60 - $100/week (unlimited messaging + live sessions) | < 1 week | None set by platform | 24/7 messaging; scheduled live video/phone sessions. | Busy schedules; commuting students; preference for digital communication. | 80-85% satisfaction; 20-30% higher continuation rates due to accessibility. |
Research indicates that 35-45% of students using mental health services access off-campus providers due to campus waitlists, session limits, or preference for continued care beyond college. Studies show treatment outcomes for off-campus care equal or exceed campus counseling, with the primary barriers being cost, averaging $100-200 per therapy session without insurance, and logistical challenges of transportation and scheduling during classes.
Community Mental Health Centers
Community mental health centers provide comprehensive services, including therapy, psychiatric medication management, case management, and crisis intervention on sliding scales based on income. Many students qualify for low-cost or free services. These centers specifically serve people without adequate insurance or financial resources. Research shows community mental health centers serve 30-35% of their clients who are students, with satisfaction rates of 75-80% comparable to private practice, despite lower costs.
Finding community centers involves searching "[your city] community mental health center" or calling 211 for local resource connections. Intake appointments typically occur within 2-4 weeks, with ongoing therapy starting shortly after. Services continue beyond college graduation, unlike campus counseling, with session limits. Studies indicate students using community mental health centers attend an average of 12-16 therapy sessions compared to 4-6 sessions in campus counseling, allowing treatment of more complex or chronic conditions.
Private Practice Therapists
Private therapists offer more flexibility in appointment times, theoretical orientations, and treatment duration compared to campus services. Student health insurance often covers mental health treatment with copays of $15-40 per session, making private practice affordable. Without insurance, therapists charge $100-200 per session, though many offer sliding scales for students. Research shows private practice therapy produces equivalent outcomes to campus counseling, with higher continuation rates of 60-70% compared to 40-50% for campus counseling.
Finding therapists involves checking your insurance provider's directory, getting referrals from campus counseling, or using directories like Psychology Today's therapist finder. Look for therapists listing specialties matching your concerns, such as anxiety, depression, trauma, relationship issues, etc. Initial sessions assess fit as therapeutic relationship quality predicts outcomes more strongly than specific techniques. Studies reveal that a strong therapeutic alliance accounts for 30-40% of treatment success.
Teletherapy and Online Counseling
Teletherapy platforms, including BetterHelp, Talkspace, and others, provide video, phone, or text-based counseling from licensed therapists. Costs range from $60-100 weekly for unlimited messaging plus live sessions. Convenience appeals to students with schedule constraints or transportation challenges. Research shows teletherapy produces equivalent outcomes to in-person therapy for most conditions, with satisfaction rates of 80-85% and continuation rates 20-30% higher than traditional therapy due to increased accessibility.
Student health insurance sometimes covers teletherapy, though coverage varies. Check with your insurance or campus health center about teletherapy options. Some campus counseling centers now offer their own teletherapy options, increasing access for commuter students or during breaks. Studies indicate that students using teletherapy average 8-10 sessions compared to 4-6 for in-person campus counseling, suggesting improved engagement through convenient access.
Peer Support and Self-Help Groups
Support groups connect people facing similar challenges, providing peer support beyond professional therapy. Groups exist for various concerns, including depression, anxiety, grief, eating disorders, substance use, and identity exploration. Organizations like NAMI offer free support groups nationwide. Research shows that support group participants report 40-50% decreased feelings of isolation and 30-40% improved coping skills even without professional therapy.
Online communities and apps provide 24/7 peer support, though quality varies and shouldn't replace professional treatment for serious conditions. Apps like Sanvello, Calm, and Headspace teach coping skills and provide mood tracking. Studies reveal that mental health apps combined with therapy improve outcomes by 20-30% compared to therapy alone, particularly for anxiety and depression management.
When Workload Triggers Mental Health Crises
Sometimes mental health crises stem partially from genuinely unsustainable academic demands rather than just mental illness. When workload consistently prevents adequate sleep, triggers severe anxiety, or makes functioning impossible despite treatment, addressing the workload itself becomes necessary. Using a reliable essay writing service for assignments in less critical courses during mental health crisis periods allows focus on recovery and high-priority coursework rather than attempting to maintain impossible standards while severely distressed.
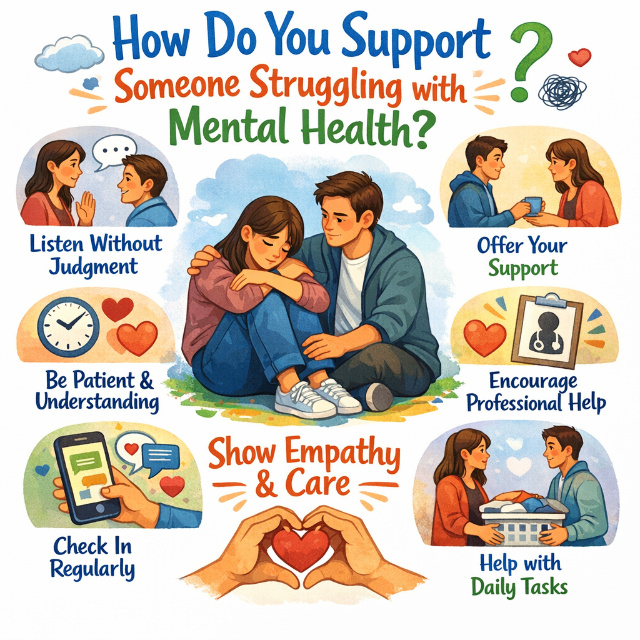
How Do You Support Someone Struggling with Mental Health?
| Support someone struggling with mental health by expressing direct concern through statements like "I've noticed you seem down lately and I'm worried about you want to talk?", listening without judgment or trying to fix problems, encouraging professional help by offering to help find resources or accompany them to appointments, checking in regularly through texts or visits showing consistent care, respecting their privacy while staying appropriately connected, recognizing warning signs of crisis including suicide mentions or severe behavior changes, and taking care of your own mental health as supporting others can be emotionally draining. |
Research shows that 70-75% of students experiencing mental health problems confide in peers before seeking professional help, making peer support crucial for connecting students to appropriate resources. Studies indicate that social support from friends predicts 30-40% better mental health outcomes, even controlling for professional treatment, though peer support should complement, not replace, professional care for serious conditions.
Expressing Concern Directly
If worried about someone, say so directly rather than hoping they'll bring it up. Use specific observations: "You've missed several classes lately and seem really stressed. Are you okay?" is more effective than vague "How are you?" Research shows that 60-70% of people experiencing mental health crises report nobody asked directly about their struggles, despite multiple people noticing concerning changes.
Avoid minimizing language like "everyone's stressed" or "it could be worse." These statements dismiss valid struggles. Instead, validate feelings: "That sounds really difficult" or "I hear you're really struggling." Studies indicate that feeling heard and validated predicts seeking help more strongly than specific advice, with 55-65% of students saying validation from friends encouraged professional help-seeking.
Listening Without Fixing
Your role is supporting, not solving. Resist urges to offer solutions or compare their problems to your own. Simply listening communicates care more effectively than advice. Research shows that people in distress rate listeners as more helpful than advice-givers by 60-70%, with being heard reducing immediate distress independent of any solutions.
Ask open-ended questions, encouraging them to share at their own pace. "How are you feeling about everything?" creates more space than "Are you depressed?" Don't pressure them to share details they're uncomfortable revealing. Studies reveal that conversation quality predicts whether people seek help afterward, with judgmental or advice-heavy conversations reducing help-seeking by 40-50% compared to validating open listening.
Encouraging Professional Help
Suggest professional resources without pushing. "Have you thought about talking to a counselor? I've heard good things about the campus counseling center," opens the door. Offer practical help like looking up phone numbers, walking with them to appointments, or sharing your own therapy experiences. Research shows that practical assistance increases help-seeking by 50-60% compared to general encouragement without specific support.
If they're resistant, respect their autonomy while staying connected. You can't force someone into treatment, but you can maintain a caring presence. Plant seeds: "I care about you, and therapy has helped me if you ever want to try it, I'll help you find someone." Studies indicate that 40-50% of students initially resistant to therapy reconsidered after trusted friends made multiple gentle suggestions over weeks or months.
Recognizing Crisis Situations
Some situations require more urgent action. If someone mentions suicide, take it seriously always. Ask directly: "Are you thinking about killing yourself?" Direct questions don't plant ideas and show you're willing to discuss difficult topics. Research shows that 75-80% of people who die by suicide communicated intent to someone beforehand, yet warning signs were often missed or dismissed.
If they confirm suicidal thoughts, don't leave them alone. Stay with them, remove means of self-harm if possible, and help connect to crisis resources, including 988 Suicide and Crisis Lifeline, Crisis Text Line at 741741, campus police, or emergency rooms. Don't promise to keep suicidal thoughts secret; getting help is more important than confidentiality. Studies show that temporary anger about confidentiality being broken is far preferable to fatal outcomes.
Setting Boundaries
Supporting struggling friends can drain you emotionally. Set boundaries around your availability and capacity. Saying "I care about you but need to focus on my own stuff right now" is both honest and appropriate. You're not responsible for someone else's mental health or recovery. Research indicates that helpers without boundaries experience 50-60% higher rates of burnout and secondary trauma compared to those maintaining healthy limits.
Encourage them to build broader support networks rather than relying entirely on you. Multiple support sources create stability and prevent any single person from bearing an excessive burden. Studies show that people with diverse support networks recover 40-50% faster from mental health crises compared to those depending on single supporters.
Key Takeaways
Mental health resources exist extensively for college students, though many remain underutilized due to stigma and lack of awareness:
- 60-70% of college students experience mental health challenges requiring professional support, with only 30-40% accessing available resources, despite 70-80% showing significant improvement within 6-8 therapy sessions
- Campus counseling provides 8-12 free sessions annually with crisis walk-in hours for urgent needs, while off-campus options include community mental health centers with sliding scales and teletherapy platforms, increasing accessibility
- Seek professional help when symptoms persist for more than 2 weeks, interfere with functioning, when experiencing any suicidal thoughts, when anxiety prevents normal activities, or when others express concern about your mood changes
- Support struggling friends by expressing direct concern, listening without judgment, encouraging professional help with practical assistance, and maintaining boundaries protecting your own wellbeing
- Mental health treatment isn't a luxury for severe cases only, it's appropriate preventive care helping students thrive rather than merely survive college
Mental health challenges are common, treatable, and not signs of weakness or failure. The pressure and stress of college create conditions where even previously healthy students develop anxiety, depression, or other conditions requiring professional support. Stigma, unfortunately, prevents many students from accessing help that would significantly improve their well-being and academic success.
If you're struggling, you deserve support. Don't wait until you're in crisis. Early intervention produces better outcomes and prevents problems from worsening. Campus and community resources exist specifically for students, with most services free or low-cost, removing financial barriers to care. Taking care of your mental health is as important as taking care of physical health and directly impacts your ability to learn, form relationships, and enjoy college. Getting support is crucial for student wellness. Similarly, academic support matters as a reliable essay writing service offers expert help to reduce stress and free up time for self-care.
When academic pressure contributes to mental health struggles by creating impossible demands, addressing both the symptoms through appropriate mental health resources and the contributing stressors through workload management protects your wellbeing more effectively than attempting to power through overwhelming distress alone. Your health and life matter more than any grade or assignment. Seeking help shows strength and self-awareness, not weakness.